Benchmarking at the national level is a helpful starting point. More actionable data are unlocked when specified for ACOs to evaluate performance across HCCs and identify opportunity within a targeted patient population. By working with CareJourney, ACOs can obtain a detailed workbook that highlights the ACO’s prevalence of medical conditions and compares recapture rates against other ACOs.
After identifying a few focus areas through our analytics, organizations can further investigate potential variability in clinical diagnosis and documentation practices within their ACO, resulting in a more accurate representation of medical complexity. If you would like a fresh look at your HCCs, please contact CareJourney today for a customized HCC benchmarking calculator.
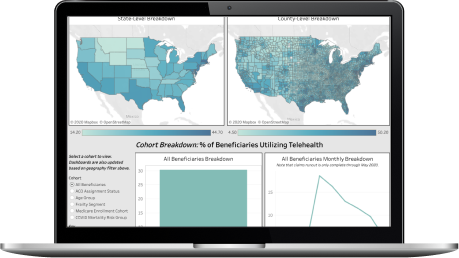
Now that you are subscribed to CareJourney JumpStart, discover more reports just like this one to see insightful metrics on other relevant topics. Or take the data further with our Population Insights tool built on the CMS-supplied CCLF files for a portfolio of clinically-relevant insights at the patient-level.
The benchmarking tool utilizes the national Medicare Fee-for-Service claims database to establish the foundation for national benchmarking. There are two main metrics: prevalence and recapture rate. The base population prevalence of medical conditions aligned to HCCs is measured as count per 1,000 members. This forms the initial benchmark of medical complexity for an ACO’s population.
The recapture rate is modeled by identifying patient diagnoses aligned to HCCs submitted on claims in the prior year (year 1) that were not submitted on claims in the most recent year (year 2). A maximum population medical complexity by HCCs was estimated by adding the medical conditions that were not recaptured to the most recent year prevalence.
Have any additional questions?
Please reach out to your main point of contact at CareJourney for more information and/or additional support regarding this analysis. If you do not have a main point of contact at CareJourney, please reach out to jumpstart@carejourney.com.
We have a large library of similar JumpStart data and custom analysis with in-depth commentary and insights on various healthcare topics.
Get access to more JumpStart dashboards to see how impactful our dataset is and what it can do to inform strategic business decisions for your organization.
CareJourney is a leading provider of clinically relevant analytics for value-based networks supporting leading payer, provider, & life sciences organizations.
Learn more about how we help organizations achieve their goals by bringing new, high-value insights out of expansive population claims data.