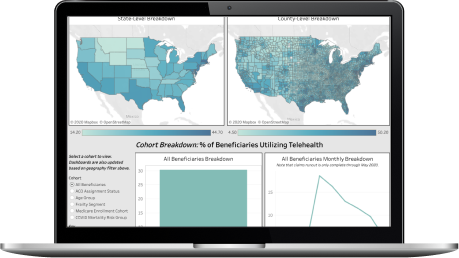
This dashboard allows users to view national level Medicare Advantage Open Enrollment changes from 2020 to 2021 as well as American Community Survey Population Indicators and Historical ACO penetration rates for the counties with a 5% or greater enrollment increase.
Use the County and State filters on the left of the dashboard to select the county that you’d like to see more details on throughout the dashboard.
Please note that changes to the filter do not modify the national KPIs.
This dashboard is based on the 100% Medicare fee-for-service claims database and the December 2020 and February 2021 MA Open Enrollment numbers.
How was information leveraged to compare the 2020 and 2021 MA Enrollment numbers?
The Dec 2020 and Feb 2021 MA Open Enrollment county level data was leveraged to compare 2020 and 2021 Enrollment.
In the county level MA vs FFS Analysis, what dataset powers the analysis?
The 2019 metrics were calculated using the 100% Medicare fee-for-service claims database in order to show historical ACO penetration and acceptance rates for a given county.
Have any additional questions?
Please reach out to your main point of contact at CareJourney for more information and/or additional support regarding this analysis. If you do not have a main point of contact at CareJourney, please reach out to jumpstart@carejourney.com.
"There was a lot of collaboration in creating this packet of market analytics, looking at which metrics would make the most sense to track. CareJourney’s process of pulling this data into a multi-layered, visual user interface replaces the manual effort previously required by our analytics team."
Mallory Cary, ACO Operations DirectorWe have a large library of similar JumpStart data and custom analysis with in-depth commentary and insights on various healthcare topics.
Get access to more JumpStart dashboards to see how impactful our dataset is and what it can do to inform strategic business decisions for your organization.
CareJourney is a leading provider of clinically relevant analytics for value-based networks supporting leading payer, provider, & life sciences organizations.
Learn more about how we help organizations achieve their goals by bringing new, high-value insights out of expansive population claims data.