Assessing Key Markets for the ET3 Model
In an effort to increase the quality of care for patients and reduce avoidable transports to the ED, the Center for Medicare and Medicaid Innovation (CMMI) developed an innovative payment model called Emergency Triage, Treat, and Transport, or ET3 for short. This model really looks to redefine emergency ground ambulance services, who until this model would only be paid by Medicare when transporting patients to approved facilities including hospitals (EDs), even if this was not the most appropriate care setting for the patient’s need.
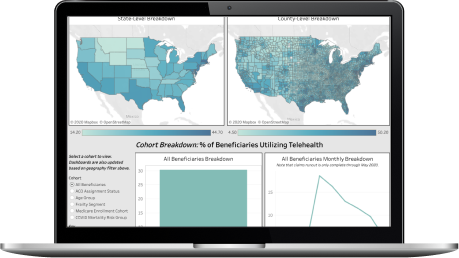
This dashboard offers insights on county-level ambulance-sourced ED claims using 2019 Medicare Fee-for-Service data. To use this dashboard, use the state and county filter to select the geographic areas you are interested in learning about.
Learn more about the ambulance-sourced avoidable ED visits, and the ET3 model on the blog!
What is the ET3 model?
Who can participate in the ET3 model?
How does CareJourney define ET3-applicable?
What is the next-step analysis to prepare me for the ET3 model?
"There was a lot of collaboration in creating this packet of market analytics, looking at which metrics would make the most sense to track. CareJourney’s process of pulling this data into a multi-layered, visual user interface replaces the manual effort previously required by our analytics team."
Mallory Cary, ACO Operations DirectorWe have a large library of similar JumpStart data and custom analysis with in-depth commentary and insights on various healthcare topics.
Get access to more JumpStart dashboards to see how impactful our dataset is and what it can do to inform strategic business decisions for your organization.
CareJourney is a leading provider of clinically relevant analytics for value-based networks supporting leading payer, provider, & life sciences organizations.
Learn more about how we help organizations achieve their goals by bringing new, high-value insights out of expansive population claims data.