Is the CMS Geographic Direct Contracting Model right for you?
What is the Geo model?
The Geo model will test whether a geographic-based approach to value-based care can improve quality of care and reduce costs from Medicare beneficiaries across the entire region leveraging a set of best practices from prior Innovative models. Geo DCEs will be taking responsibility for the total cost of care for a set of Medicare beneficiaries in an entire region, thereby encouraging DCEs to partner with community organizations in a given region to create the most effective care network.
How were the CBSA chosen for the dashboard?
The 15 CBSA are candidate regions announced by CMS and can be found here
What is the definition of "eligible"?
Eligible beneficiaries includes beneficiaries who meet all of the following criteria:
What is the definition of "aligned"?
Aligned beneficiaries are beneficiaries that meet the Eligibility criteria mentioned above and have received a PQEM or Primary Care service within the alignment timeframe.
Please refer to Appendix B: Beneficiary Alignment Procedures of the Financial Guide for additional detail regarding beneficiary alignment.
What is the definition of "unaligned"?
Unaligned beneficiaries are beneficiaries that meet the Eligibility criteria mentioned above, but have not received a PQEM or Primary Care service within the alignment timeframe.
Please refer to Appendix B: Beneficiary Alignment Procedures of the Financial Guide for additional detail regarding beneficiary alignment.
What does the PBPM calculation include?
The Per Beneficiary Per Month (PBPM) calculation includes Part B, Inpatient, Outpatient, Home Health, Skilled Nursing Facility, Hospice, and DME.
What HCC risk score is this analysis using?
The Average Adjusted HCC Score is based on the CMS-HCC Non-ESRD Perspective v22 model.
I want a more in-depth analysis to evaluate my readiness for this model, what should I do?
Please reach out to your main point of contact at CareJourney for more information and/or additional support regarding applying for the Geo model. If you do not have a main point of contact at CareJourney, please reach out to jumpstart@carejourney.com.
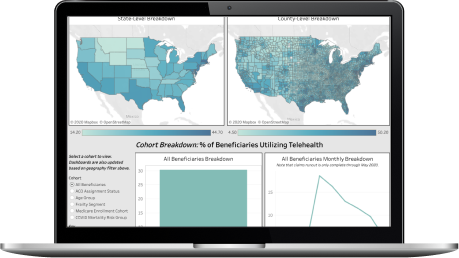
"There was a lot of collaboration in creating this packet of market analytics, looking at which metrics would make the most sense to track. CareJourney’s process of pulling this data into a multi-layered, visual user interface replaces the manual effort previously required by our analytics team."
Mallory Cary, ACO Operations DirectorWe have a large library of similar JumpStart data and custom analysis with in-depth commentary and insights on various healthcare topics.
Get access to more JumpStart dashboards to see how impactful our dataset is and what it can do to inform strategic business decisions for your organization.
CareJourney is a leading provider of clinically relevant analytics for value-based networks supporting leading payer, provider, & life sciences organizations.
Learn more about how we help organizations achieve their goals by bringing new, high-value insights out of expansive population claims data.